Current Issue
Mesalamine (5-ASA) Induced Myocarditis: A Case Report
Avi Kaul1, Frank M Iacovone2, Sameer Kaul2,*, Marc S Fisk2
1Division of Cardiology, Department of Internal Medicine, Clara Maass Medical Center, Robert Wood Johnson University, Barnabas Health System (RWJBH), USA
2Department of Cardiology, Clara Maass Medical Centre, Belleville, New Jersey, USA
*Corresponding author: Sameer Kaul, Department of Cardiology, Clara Maass Medical Centre, Belleville, New Jersey, USA, Tel: 9734502000, E-mails: [email protected]; [email protected]
Received Date: May 13, 2025
Publication Date: May 30, 2025
Citation: Kaul A, et al. (2025). Mesalamine (5-ASA) Induced Myocarditis: A Case Report. Cases. 4(2):22.
Copyright: Kaul A, et al. © (2025).
ABSTRACT
Myocarditis is a rare complication linked to Mesalamine therapy, a medication commonly prescribed for treating inflammatory bowel disease. Mesalamine-induced myocarditis may be more prevalent than previously believed. This case is an important example of why physicians must be aware of Mesalamine treatment, a relatively common first-line drug for patients with Inflammatory bowel diseases. The cardiac side effects of this drug can present as Myocarditis and can lead to significant morbidity if not identified early. Stopping the drug and early treatment can result in good outcomes, as in the given case. A 51-year-old male who was diagnosed with ulcerative colitis developed myocarditis 21 days after the initiation of mesalamine therapy. He presented to the emergency room with difficulty breathing. Labs revealed elevated high-sensitivity Troponins. An echocardiogram showed reduced Left Ventricular function. The echo revealed moderate to severe global hypokinesis of the left ventricle. Subsequent urgent cardiac catheterization revealed normal right and left Coronaries with no obstruction. Normal coronaries in the setting significantly elevated Troponins led to the diagnosis of myocarditis. After stopping mesalamine, the patient's symptoms and left ventricular function improved rapidly, and he recovered fully.
Categories: Cardiology, Gastroenterology, Emergency Medicine.
Keywords: Mesalamine, Myocarditis, Ulcerative Colitis.
INTRODUCTION
Inflammatory bowel disease (IBD) is a chronic disorder that presents with intermittent episodes of exacerbation and is classified into Crohn's disease (CD) and Ulcerative colitis (UC).
Ulcerative colitis (UC) is a chronic inflammatory condition of unclear etiology affecting the large bowel, most commonly the rectum, and extending proximally continuously.
Crohn's disease (CD) can cause inflammation anywhere from the mouth to the anus in the gastrointestinal tract.
Mesalamine, chemically known as 5-aminosalicylic acid (5-ASA), belongs to the group of drugs known as amino salicylates. It is typically prescribed as first-line medical therapy in treating UC [1-3]. The precise mechanism of its action is currently not well understood.
It is hypothesized that it regulates the inflammatory response from the cyclooxygenase and lipoxygenase pathways, thereby reducing the production of prostaglandins and leukotrienes.
Alternative possible mechanisms involve disrupting the production of inflammatory cytokines by lowering the activity of nuclear factor kappa light chain enhancer of activated B cells (NF-κB).
This reduction can lead to the inhibition of tumor necrosis factor (TNF), which plays a crucial role in the inflammatory response. Additionally, these mechanisms can affect the cellular functions of various immune components, including mucosal lymphocytes, macrophages, and natural killer cells, thereby impacting the overall immune response and inflammation regulation within the body.
Mesalamine is thought to function as a free radical scavenger and an antioxidant [4,5].
Mesalamine is approved by the FDA for both the induction and maintenance of remission in ulcerative colitis (UC). It is typically used for patients with mildly to moderately active ulcerative colitis (UC). The off-label use of mesalamine now encompasses the treatment of Crohn’s disease (CD) in patients who have undergone surgical resection of the affected sections of the bowel. It is available in both capsule and tablet forms, allowing for flexibility in administration. Patients can take mesalamine with or without food, making it convenient to integrate into their daily routines. It can also be administered rectally in the form of an enema, foam, or suppository.
Patients typically demonstrate good tolerance to most formulations of mesalamine. Nevertheless, it is important to recognize that adverse effects may occur, which can include nausea, gastrointestinal disturbances, abdominal pain, headaches, nasopharyngitis, skin rash, arthralgias, agranulocytosis, aplastic anemia, myalgias, bone marrow suppression, oligospermia, hematuria, and cholestatic hepatitis. Renal impairment, which includes interstitial nephritis, nephrotic syndrome, and renal failure, necessitates careful monitoring of the patient before and during treatment [6].
The use of this medication is contraindicated in individuals with severe liver or kidney impairment, as well as in those who have existing gastric or duodenal ulcers.
Myocarditis is an uncommon yet acknowledged complication of mesalamine, with the potential to progress and lead to cardiogenic shock and, ultimately, death [7].
It is postulated that Mesalamine causes myocarditis via a cell-mediated hypersensitivity reaction.
Our case report outlines the presentation of a 51-year-old male with myocarditis induced by Mesalamine.
CASE REPORT
A 51-year-old man who had been newly diagnosed with Ulcerative Colitis (UC) three weeks before admission. Three weeks ago, he was started on 800mg of Mesalamine three times daily and 5mg of Prednisone daily for the treatment of UC. The patient was admitted to the Emergency Department with complaints of chest pain and difficulty breathing, which started a few days prior with progression to SOB on minimal exertion, which prompted the ER visit. He also reported ongoing diarrhea in association with their UC diagnosis three weeks before admission.
The patient's medical history includes hypertension, hypothyroidism, and hyperlipidemia. There is no history of any significant past surgeries. The patient has no known allergies and denies smoking, alcohol consumption, or use of illicit drugs. He works as a truck driver.
Although the patient has no history of heart disease, his father had a history of heart failure at the age of 53.
His current home medications include Losartan (50mg oral tablet), Pantoprazole (40mg oral tablet), Levothyroxine (25 mcg oral tablet), and Metoprolol Succinate ER (25mg oral tablet).
During the physical examination, no unusual findings were observed except for tachycardia. Upon admission, laboratory tests revealed an elevated Troponin HS level of 3,626 mcg/L (normal range ≤58). The electrocardiogram (EKG) showed normal sinus rhythm. The Erythrocyte sedimentation rate (ESR) was elevated at 128mm/hr.
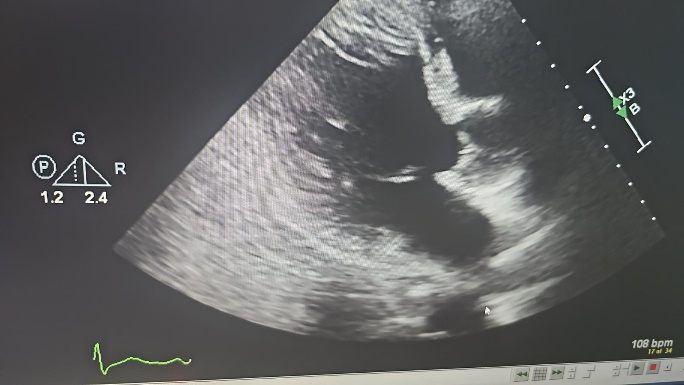
Cardiac catheterization was performed due to suspicion of non-ST-elevation myocardial infarction (NSTEMI) with significantly elevated troponins, but it revealed normal coronary arteries. An echocardiogram (Echo) showed moderate to severe global hypokinesis of the left ventricle, consistent with systolic dysfunction associated with increased left atrial pressure. The ejection fraction (EF) was found to be low, ranging between 30% and 35%, compared to the normal range of 55% and above.
His chest X-ray and chest computed tomography (CT) yielded normal results. Abdominal computed tomography (CT) revealed pancolitis. The results for the hepatitis virus panel, HIV tests, and QuantiFERON (QFT) test for Tuberculosis were all negative. Stool cultures for Salmonella, Shigella, Campylobacter, E. coli O:157, and Shiga toxin-producing E. coli revealed no growth.
The results of the antinuclear antibody (ANA) screen using IFA and urine toxicology were all negative. The patient tested negative for SARS-CoV-2 Rapid, Influenza A, Influenza B, C. difficile, and 027-NAP1.
Further considerations included the possibility of a vasculitis or autoimmune process, viral myocarditis, and extraintestinal manifestations of IBD. The patient had no previous signs of underlying infection and was in good systemic health, including no other physical or skin stigmata, ruling out vasculitis or autoimmune processes. Typically, extraintestinal symptoms of IBD manifest years after diagnosis. However, in this case, the patient experienced symptoms shortly after initiating a new drug therapy, indicating that Mesalamine was likely the cause.
Following a thorough evaluation of the findings, the patient was given a provisional diagnosis of acute myocarditis.
The patient was treated conservatively with a beta blocker and ACE inhibitor for HFrEF (heart failure with reduced ejection fraction), and the administration of mesalamine was promptly discontinued.
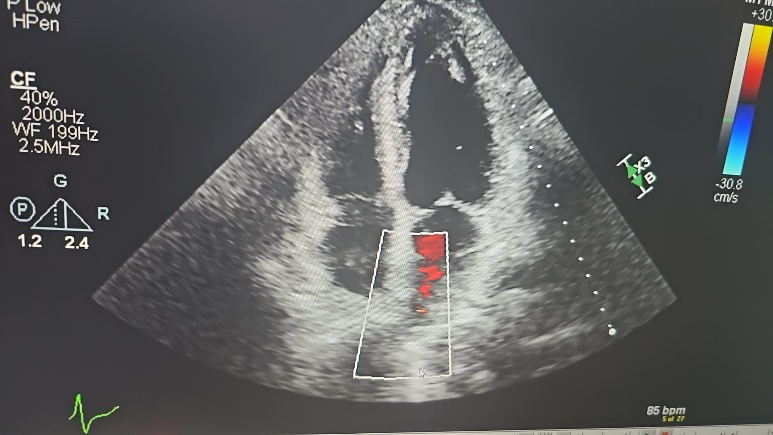
The diagnosis of Mesalamine-induced myocarditis was confirmed by the gradual improvement in the patient's condition after discontinuation of the drug, with both ischemic and infectious workups returning negative results. This improvement was shown by the increase in ejection fraction on the echocardiogram, rising from 30-35% at admission to 50-55% by day 7.
Additionally, there was a significant decrease in the Troponin levels from 3,626 mcg/L at admission to 276 mcg/L on day 7. He was discharged home in a stable condition.
A subsequent echocardiogram two months later revealed complete normalization of LV function to 55-60%, falling within the normal range. The observations were consistent with the resolution of a myocarditis episode, and the patient subsequently achieved a complete recovery.
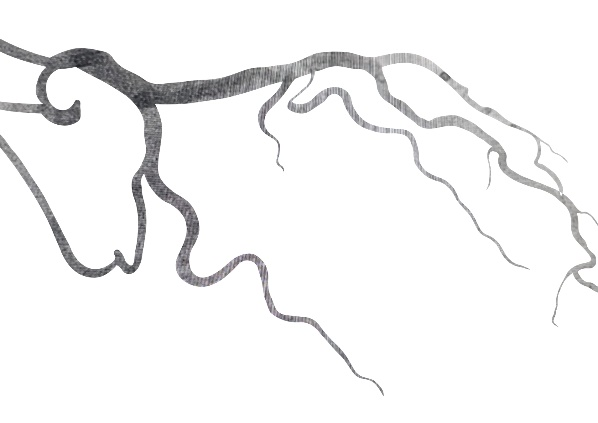
Cardiac catheterization done on 04/02/2023 revealed normal coronary arteries.
Figure 1,2. Right coronary artery 2: Left system with left main giving rise to Left anterior descending artery and Left Circumflex artery.
Figure 3,4,5. ECHO done on 04/04/2023 on admission, figure 3 parasternal long axis view, figure 4 short axis view, figure 5. Apical 4-chamber view showing low ejection fraction.
ECHO done on 06/27/2023 after stopping Mesalamine.
Figure 6. Short axis view. Figure 7. Apical 4-chamber view.
DISCUSSION
Cardiac disorders may be linked to inflammatory bowel disease (IBD) or may result from the side effects of medication. Several hundred cases of pericarditis and perimyocarditis have been documented in the scientific literature [8]. In fact, up to one-third of patients with IBD may develop myocarditis during their disease, and this can be clinically indistinguishable from 5-ASA-induced myocarditis [9].
Myocarditis is a rare but potentially life-threatening side effect of 5-ASA therapy, typically occurring 2 to 4 weeks after starting treatment [9,10].
While the precise mechanism remains uncertain, it is theorized that myocarditis results from cell-mediated hypersensitivity, a hypothesis deemed more reasonable than the notion of a direct cardiotoxic effect of the drug [7].
Research indicates that discontinuing 5-ASA medication is effective in resolving cardiac complications, providing additional evidence for a hypersensitivity reaction [11,12].
However, diagnosing myocarditis induced by 5-ASA is notably challenging due to the absence of specific laboratory or cardiac imaging findings that are pathognomonic for this condition. The crucial aspects to identify include the emergence of cardiac symptoms like chest pain, dyspnea, or fever shortly after initiating the medication, typically occurring within 28 days.
Noninvasive imaging techniques such as echocardiography and cardiovascular magnetic resonance (CMR) show a high diagnostic yield. They can be alternatives to myocardial biopsy, which, although considered the standard, is rarely performed due to safety concerns [13,14].
Medication discontinuation is necessary, and other potential causes of myocarditis, such as viral myocarditis, vasculitis, or extraintestinal manifestations of IBD, should be ruled out [15-18].
CONCLUSION
As evidenced by our patient's case, physicians need to recognize this rare but potentially life-threatening adverse effect of mesalamine, especially given its widespread use for treating inflammatory bowel disease. It is crucial to include myocarditis in the range of potential diagnoses for chest pain in a patient using mesalamine, as the recommended course of action involves discontinuing the medication. This typically results in a rapid improvement of symptoms within 24 hours without causing any lasting sequelae.
ABBREVIATIONS
5-ASA: Mesalamine or 5-Aminosalicylic Acid; IBD: Inflammatory Bowel Disease; UC: Ulcerative Colitis; CD: Crohn’s Disease.
FUNDING
Not Applicable.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient to publish this case report and any accompanying images.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
COMPETING INTERESTS
None.
ACKNOWLEDGMENTS
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
AUTHOR’S CONTRIBUTION
All authors contributed to drafting, revising, reading, and approving the final manuscript.
REFERENCES
- Nakashima J, Preuss CV. (2023). Mesalamine (USAN). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available at: https:// www.ncbi.nlm.nih.gov/books/NBK551714/
- Bergman R, Parkes M. (2006). Systematic review: the use of mesalazine in inflammatory bowel disease. Aliment Pharmacol Ther. 23(7):841-855.
- Conrad K, Roggenbuck D, Laass MW. (2014). Diagnosis and classification of ulcerative colitis. Autoimmun Rev. 13(4-5):463-466.
- Drugs and Lactation Database (LactMed®). (2023). National Institute of Child Health and Human Development; Bethesda (MD). Mesalamine.
- Garud S, Peppercorn MA. (2009). Ulcerative colitis: current treatment strategies and future prospects. Therap Adv Gastroenterol. 2(2):99-108.
- Ham M, Moss AC. (2012). Mesalamine in the treatment and maintenance of remission of ulcerative colitis. Expert Rev Clin Pharmacol. 5(2):113-123.
- Meier J, Sturm A. (2011). Current treatment of ulcerative colitis. World J Gastroenterol. 17(27):3204-3212.
- Sehgal P, Colombel JF, Aboubakr A, Narula N. (2018). Systematic review: safety of mesalazine in ulcerative colitis. Aliment Pharmacol Ther. 47(12):1597-1609.
- Freeman HJ, Salh B. (2010). Recurrent myopericarditis with extensive ulcerative colitis. Can J Cardiol. 26(10):549-550.
- Rellecke P, Strauer BE. (2006). Chronic Inflammatory bowel disease and cardiovascular complications [in German]. Med Klin (Munich). 101(Suppl 1):56-60.
- Moss AC, Peppercorn MA. (2007). The risks and the benefits of mesalazine as a treatment for ulcerative colitis. Expert Opin Drug Saf. 6(2):99-107.
- Cooper LT Jr. (2009). Myocarditis. N Engl J Med. 360(15):1526-1538.
- Liu Y, Ye J, Zhu J, Chen W, Sun Y. (2012). Myocarditis due to mesalamine treatment in a patient with Crohn’s disease in China. Turk J Gastroenterol. 23(3):304-346.
- Doganay L, Akinci B, Pekel N, Simsek I, Akpinar H. (2006). Mesalazine-induced myopericarditis in a patient with ulcerative colitis. Int J Colorectal Dis. 21(2):199-200.
- Radhakrishnan ST, Mohanaruban A, Hoque S. (2018). Mesalazine-induced myocarditis: a case report. J Med Case Rep. 12(1):44.
- Brown G. (2016). 5-Aminosalicylic acid-associated myocarditis and pericarditis: a narrative review,Can J Hosp Pharm. 69(6):466-472.
- Biesbroek PS, Hirsch A, Zweerink A, van de Ven PM, Beek AM, Groenink M, et al. (2017). Additional diagnostic value of CMR to the European Society of Cardiology (ESC) position statement criteria in a large clinical population of patients with suspected myocarditis. Eur Heart J Cardiovasc Imaging. 19(12):1397-1407.
- Dominguez F, Kuhl U, Pieske B, Garcia-Parvia P, Tschope C. (2016). Update on myocarditis and inflammatory cardiomyopathy: reemergence of endomyocardial biopsy. Rev Esp Cardiol. 69(2):178-187.
 Abstract
Abstract  PDF
PDF