Current Issue
A Rare Cause of Intestinal Obstruction in a Newborn: Anomalous Congenital Band
A Ayad*, S Sghir, M Bahous, R Abilkassem
Neonatal Intensive Care Unit, Military Hospital of Rabat, Morocco
*Corresponding author: Dr. Ayad Anass, Neonatal Intensive Care Unit, Military Hospital of Rabat, University Mohamed V of Rabat, Hay Riad, 1000, Rabat, Morocco, Phone: +212661315979, E-mail: [email protected]
Received Date: August 28, 2025
Publication Date: September 12, 2025
Citation: Ayad A, et al. (2025). A Rare Cause of Intestinal Obstruction in a Newborn: Anomalous Congenital Band. Cases. 4(2):24.
Copyright: Ayad A, et al. © (2025).
ABSTRACT
Anomalous congenital bands (ACBs) are rare anatomical anomalies that can cause acute intestinal obstruction in neonates and infants. Early recognition is critical as delayed diagnosis may lead to bowel ischemia or death. We report the case of a 5-day-old full-term newborn with progressive abdominal distension, bilious vomiting, and failure to pass stool. Radiological evaluation revealed duodenal obstruction, and surgical exploration identified a congenital fibrous band compressing the ileum. The band was excised, preserving bowel continuity, and the infant had an uneventful recovery. Clinicians should suspect ACBs in neonates with unexplained intestinal obstruction, as prompt surgical management can be lifesaving. Anomalous congenital bands (ACBs) are rare anatomical anomalies that can cause acute intestinal obstruction in neonates and infants. Their preoperative diagnosis is often challenging due to nonspecific clinical features and the absence of prior surgical history. We report the case of a 5-day-old full-term newborn who presented with signs of intestinal obstruction. Clinical evaluation revealed abdominal distension, bilious gastric residues, and absence of meconium passage. Abdominal radiography demonstrated air-fluid levels suggestive of small bowel obstruction. Surgical exploration revealed an anomalous congenital band compressing a segment of ileum, resulting in a mechanical obstruction. The band was resected, and an ileo-ileal end-to-end anastomosis was performed following resection of a dilated aperistaltic bowel segment. Postoperative recovery was uneventful.
Keywords: Anomalous Congenital Band, Neonatal Intestinal Obstruction, Bilious Vomiting, Congenital Bowel Anomalies, Neonatal Surgery
INTRODUCTION
Neonatal intestinal obstruction is a potentially life-threatening condition with a broad spectrum of etiologies. While the most common causes include intestinal atresia, malrotation with volvulus, Hirschsprung’s disease, and meconium-related disorders, extrinsic causes such as congenital bands are far less frequent. Anomalous congenital bands (ACBs) are rare remnants of embryonic structures, possibly arising from persistent fetal vessels or ventral mesenteric folds that fail to regress [1,2].
These bands can compress the bowel externally and lead to partial or complete obstruction. In this report, we present a case of a 5-day-old newborn with acute intestinal obstruction caused by a congenital band, and we discuss the clinical presentation, surgical findings, and management in the context of available pediatric literature.
CASE REPORT
A 5-day-old male newborn was admitted to the neonatal intensive care unit for abdominal distension, decreased feeding, and progressive bilious vomiting. He was born at term from an uneventful pregnancy, with normal antenatal ultrasounds. Birth weight was 2800 g, Apgar scores were 10 at 5 min, and meconium was passed within the first 24 h of life.
Timeline of symptoms:
• Day 1: Normal adaptation, meconium passed.
• Day 2: Reduced feeding frequency noted.
• Day 3: Onset of mild abdominal distension.
• Day 4: Bilious vomiting and worsening distension prompted hospital admission.
• Day 5: Contrast study revealed duodenal obstruction → surgical intervention performed.
On admission: The newborn was hemodynamically stable (HR 145 bpm, RR 26/min, T 37.6°C, BP 75/48 mmHg) with mild dehydration. Lab work: leukocytes 15 × 10³/μL, Hb 12.5 g/dL, platelets 185 × 10³/μL, electrolytes normal. Nasogastric tube drainage yielded bilious residues; rectum was empty. Resuscitation: IV fluids, nasogastric decompression, and perioperative antibiotics were initiated.
Surgery: Exploratory laparotomy revealed a fibrous congenital band compressing the ileum without ischemia or atresia. The band was divided, bowel viability confirmed, no resection required. Postoperative course: Full oral feeds resumed by the fourth postoperative day, discharge on day 10 with normal bowel function.
A 5-day-old male newborn was admitted to the neonatal intensive care unit for abdominal distension, decreased feeding frequency, and generalized hypotonia. He was born at term from a well-followed pregnancy with no reported prenatal abnormalities. Antenatal ultrasound was normal, and maternal laboratory results were unremarkable. Delivery was vaginal, with a birth weight of 2800 g and Apgar scores of 10 at the fifth minute. Meconium was passed within the first 24 hours of life.
Over the following days, the infant developed progressive abdominal distension, significant bilious vomiting, and intermittent episodes of abdominal colic. Upon admission, the newborn was hemodynamically stable: heart rate was 145 bpm, respirations 26 per minute, temperature 37,6blood pressure was 75/48 mmHg, and capillary blood glucose was within normal limits. He weighed 2650 g, with mild clinical signs of dehydration. Nasogastric aspiration revealed clearly bilious residue. Rectal ampulla was empty.
Parenteral solutions were started. Complete blood count with leukocytes 15x103/μL, segmental neutrophils 89, hemoglobin was 12,5g/dL, hematocrit 50%, platelets 185 185/103/μL, there was no important electrolyte imbalance in the blood chemistry.
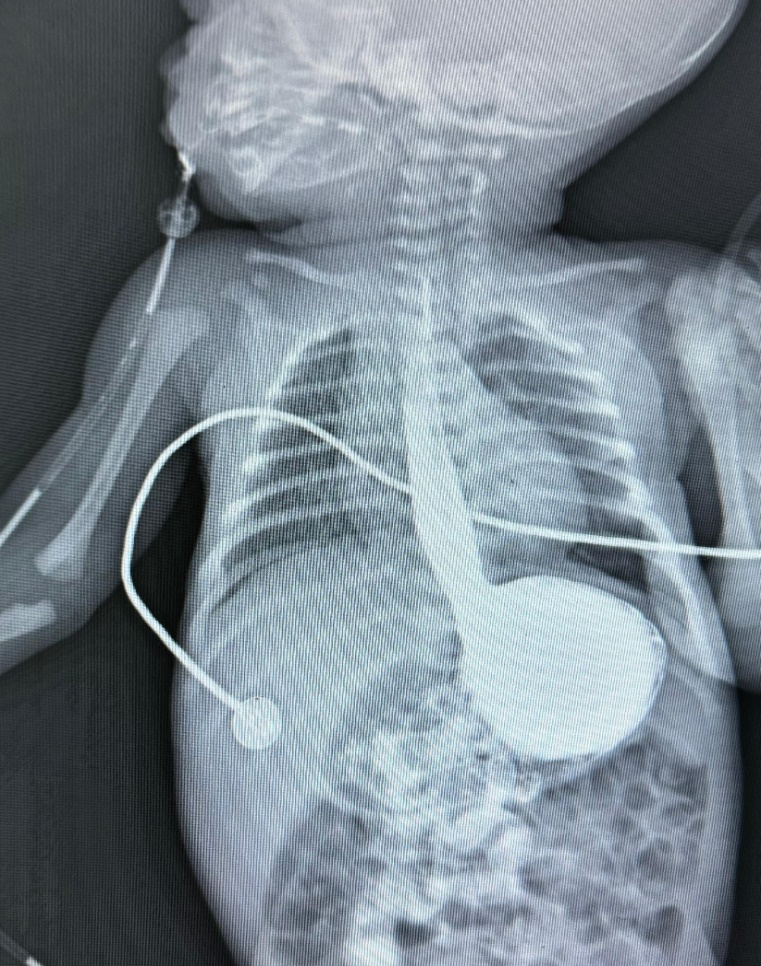
In light of suspected neonatal intestinal obstruction, a contrast study with barium was performed (Figure1). The abdominal X-ray revealed a markedly distended stomach and proximal duodenum with an abrupt cut-off, and no contrast passage beyond the second portion of the duodenum—findings suggestive of a duodenal obstruction, likely from an extrinsic cause.
The newborn was taken to the operating room for exploratory laparotomy. Intraoperative findings revealed a congenital fibrous band compressing the small intestine (Figure 2).
No signs of intestinal necrosis were observed. The band was surgically excised, Intestinal integrity and passage were intact and not disrupted by excision of band. No remnant of omphalomesenteric canal was found. On postoperative forth day, patient was fed through nasogastric tube.
On postoperative fifth day, patient was fed wholly through oral route. Patient was discharged on postoperative10th day with oral intake and spontaneous defecation.
Figure 1. Contrast radiograph showing abrupt duodenal obstruction (arrow).
Figure 2. Intraoperative image revealing the congenital fibrous band (arrow).
Congenital bands are an uncommon but important cause of neonatal intestinal obstruction. While most neonatal obstructions arise from intrinsic anomalies such as atresia or malrotation, ACBs represent a rare extrinsic cause, often diagnosed intraoperatively due to nonspecific clinical and imaging findings. Our case is notable for presentation at day 5 of life with duodenal-level obstruction but no ischemia, and successful outcome with simple band excision.
Literature review shows variable age at presentation, ranging from neonatal period to adulthood. Recent case series confirm the small intestine as the most frequent site, with duodenal involvement less common but clinically significant. Early surgery prevents complications such as necrosis or perforation. Our findings align with contemporary reports emphasizing prompt exploration when intrinsic causes are excluded and obstruction persists.
DISCUSSION
Congenital bands are rare but significant causes of intestinal obstruction in the pediatric population. These fibrous structures, believed to be remnants of embryonic vessels or mesenteric folds, may cause extrinsic compression of the bowel, leading to partial or complete obstruction without prior surgical history [1,3,4]. While most cases of neonatal intestinal obstruction are attributable to intrinsic anomalies such as atresia, stenosis, or malrotation [2,5], anomalous congenital bands (ACBs) remain an under-recognized etiology, particularly in neonates [3,6].
In our case, a 5-day-old term neonate presented with progressive abdominal distension, bilious vomiting, and signs of intestinal colic, following normal antenatal evaluations and unremarkable early neonatal adaptation. The presence of bilious nasogastric residue, empty rectal ampulla, and a contrast study showing duodenal-level obstruction pointed to a mechanical etiology. Exploratory surgery confirmed the presence of a congenital fibrous band compressing a segment of the small bowel, without associated atresia or ischemia.
ACBs can be located anywhere along the gastrointestinal tract but are more commonly reported in the small intestine, particularly the jejunum and ileum [3,6,7]. Duodenal involvement, although less frequent, has been described and often mimics more common causes such as annular pancreas or Ladd’s bands associated with malrotation [1,2,5]. In the neonatal period, early diagnosis is essential to avoid complications such as bowel necrosis, perforation, or even death [8,9].
The clinical presentation of ACBs is nonspecific and indistinguishable from other causes of neonatal intestinal obstruction. Radiological findings may show a level of obstruction but rarely identify the band itself. Therefore, the diagnosis is typically made intraoperatively [3,4,10]. In our case, the absence of signs of ischemia allowed for simple excision of the band without bowel resection, highlighting the importance of early surgical intervention.
A review of the literature reveals that ACBs can present at any age—from neonates to adults—with variable clinical manifestations ranging from intermittent abdominal pain to acute surgical abdomen [6,7,11]. Several fatal cases have also been reported due to delayed diagnosis or intestinal ischemia [8,12]. Thus, in any neonate presenting with signs of mechanical obstruction without prior surgery or classical intrinsic causes, ACBs should be considered in the differential diagnosis.
In neonates with unexplained intestinal obstruction and no intrinsic cause, anomalous congenital bands should be suspected. Prompt surgical exploration enables definitive diagnosis, prevents ischemic complications, and ensures excellent outcomes [13,14].
CONCLUSION
Anomalous congenital bands, although rare, should not be overlooked as a potential cause of intestinal obstruction in neonates. Given the absence of pathognomonic clinical or radiological signs, a high index of suspicion is essential, especially when other common etiologies are excluded. Early surgical exploration remains the definitive diagnostic and therapeutic approach. Awareness of this condition among neonatologists, pediatric surgeons, and radiologists is vital to ensure prompt management and favorable outcomes.
CONFLICTS OF INTEREST AND FUNDING
The authors declare that they have no conflicts of interest related to this case report. No external funding or financial support was received for the preparation of this manuscript.
REFERENCES
- Crankson SJ, Al-Mane KA, Al-Zaben A, Al-Dhafian A. (2000). Extrinsic duodenal obstruction from anomalous congenital band. Ann Saudi Med. 20(5-6):443–444.
- Applebaum H, Sydorak R. (2012). Duodenal atresia and stenosis–annular pancreas. In: Coran AG, Adzick NS, Krummel TM, Laberge JM, Shamberger RC, Caldamone AA, editors. PediatricSurgery. 7th ed. Elsevier Inc.
- Erginel B, Soysal FG, Ozbey H, Keskin E, Celik A, Karadag A, et al. (2016). Small Bowel Obstruction due to Anomalous Congenital Bands in Children. Gastroenterol Res Pract. 2016:7364329.
- Akgür FM, Tanyel FC, Büyükpamukçu N, Hiçsönmez A. (1992). Anomalous congenital bands causing intestinal obstruction in children. J Pediatr Surg. 27(4):471-473.
- Wayne ER, Burrington JD. (1973). Extrinsic duodenal obstruction in children. Surg Gynecol Obstet. 136(1):87-91.
- Sarkar D, Gongidi P, Presenza T, Scattergood E. (2012). Intestinal obstruction from congenital bands at the proximal jejunum: a case report and literature review. J Clin Imaging Sci 2:78.
- Yang KH, Lee TB, Lee SH, Kim SH, Cho YH, Kim HY. (2016). Congenital adhesion band causing small bowel obstruction: What's the difference in various age groups, pediatric and adult patients? BMC Surg. 16(1):79.
- Maiese A, Bonaccorso L, Dell'Aquila M, Gitto L, Bolino G. (2013). Anomalous congenital band and intestinal obstruction: report of a fatal case in a child. Forensic Sci Med Pathol. 9(4):588-590.
- Nouira F, Sarrai N, Charieg A, Jlidi S, Chaouachi B. (2012). Small bowel obstruction by an anomalous congenital band. Acta Chir Belg. 112(1):77-78.
- Galván-Montaño A, Trejo-Ávila M, García-Moreno S, Pérez González A. Banda congénita anómala una patología rara de obstrucción intestinal en niños. Caso clínico [Congenital anomaly band, a rare cause of intestinal obstruction in children. Case report]. Cir Cir. 85(2):164-167.
- Fang AC, Carnell J, Stein JC. (2012). Constipation in a 7-year-old boy: congenital band causing a strangulated small bowel and pulseless electrical activity. J Emerg Med. 42(3):283-287.
- Tsukuda K, Watanabe K, Nakahara S, Tada A. (2009). A case of a pediatric intraabdominal hemorrhage caused by anomalous congenital band. Jpn J Gastroenterol Surg. 42(12):1626-1630.
- Sannananja B, Shah H, Avhad G, Agrawal A. (2016). Unusual case of an anomalous congenital band causing acute small bowel obstruction in a case of abdominal tuberculosis. J Mahatma Gandhi Inst Med Sci. 21(2):82.
- Miyao M, Takahashi T, Uchida E. (2017). A case of anomalous congenital band that was difficult to differentiate from omphalomesenteric duct anomaly. J Nippon Med Sch. 84(5):304-307.
 Abstract
Abstract  PDF
PDF