Past Issues
Ooid and Aligned-Intranodal Palisaded Myofibroblastoma
Anubha Bajaj*
Consultant Histopathologist, AB Diagnostics, India
*Corresponding Author: Anubha Bajaj, Consultant Histopathologist, AB Diagnostics, India; Email: [email protected]
Received Date: April 6, 2023
Publication Date: May 16, 2023
Citation: Bajaj A. (2023). Ooid and Aligned-Intranodal Palisaded Myofibroblastoma. Cases. 2(2):10.
Copyright: Bajaj A. © (2023).
ABSTRACT
Intranodal palisaded myofbroblastoma is an uncommon, benign neoplasm arising within lymph nodes and commonly incriminates inguinal lymph nodes. Of obscure pathogenesis, intranodal palisaded myofibrobastoma may concur with overexpression of cyclin D1 or viral oncogenesis and manifests as a painless, gradually progressive tumefaction. Pathognomonic morphological features appear as proliferation of spindle shaped cells with nuclear palisading, a collagenous pseudo-capsule and compressed circumscribing peripheral lymph node tissue. Also, amianthoid fibres delineating fine, peripheral spokes, focal pauci-cellular zones and extracellular or intracellular fuchsinophilic bodies may be discerned.
Keywords: Lymph node, palisaded, amianthiod
INTRODUCTION
Intranodal palisaded myofbroblastoma is an infrequently discerned, benign neoplasm arising within lymph nodes. Tumefaction is comprised of myoid or myofibroblastic spindle shaped cells demonstrating a focal palisaded pattern accompanied by ‘amianthoid’ fibres. Tumefaction simulates schwannoma and is additionally designated as intranodal haemorrhagic spindle cell tumour with amianthoid fibres. Previously denominated as intranodal schwannoma, the neoplasm was initially scripted by Weiss et al and Suster et al in 1989 [1,2]. Amianthoid simulates amianthus or fine asbestos fibres wherein tumour fibres appear reminiscent of amianthoid fibres. Nevertheless, constituent fibres are composed of collagen fibres of normal thickness, in contrast to thick collagen fibres comprising ‘true’ amianthoid fibres. The exceptional intranodal palisaded myofibroblastoma commonly arises within adult, middle aged population wherein majority (65%) of individuals between 45 years to 55 years may display the neoplasm. A male predominance is observed with male to female proportion of 2:1. A specific ethnic predisposition is absent [3,4]. Intranodal palisaded myofibroblastoma commonly incriminates inguinal lymph nodes. Besides, neoplasm is documented to emerge within the retroperitoneum [3,4]. Of obscure pathogenesis, intranodal palisaded myofibrobastoma may be engendered in association with overexpression of cyclin D1. Additionally, viral oncogenesis may induce the neoplasm. Intranodal palisaded myofibroblastoma manifests as a painless, gradually progressive tumefaction [3,4].
Upon gross examination, a well circumscribed, grey/white tumour nodule is encountered. Foci of haemorrhage may be discerned. The nodule is circumscribed by peripherally disseminated lymph node tissue [4,5].
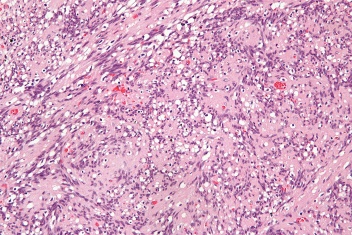
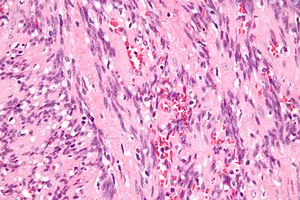
Upon cytological examination, the neoplasm is moderately cellular and is composed with benign, dissociated or singular spindle shaped cells pervaded with elongated nuclei with pointed ends. Occasional twisted nuclei may be observed. The cellular component is embedded within a pale, fibrillary matrix impregnated with hemosiderin granules. Cellular atypia is generally absent [4,5]. Upon microscopy, the neoplasm manifests pathognomonic features as ~proliferation of spindle shaped cells which characteristically demonstrate nuclear palisading. Foci of haemorrhage may circumscribe spindle shaped cellular component. A collagenous pseudo-capsule encompasses the neoplasm. The gradually progressive tumour nodule compresses peripheral lymph node tissue wherein peripheral rim of lymphoid tissue manifests as a remnant of lymph node. ~bland, spindle shaped tumour cells manifest with foci of nuclear palisading ~intra-parenchymal haemorrhage and extravasation of red blood cells may ensue ~amianthoid fibres configure vascular articulations encompassed with collagen fibres delineating fine, peripheral spokes ~focal pauci-cellular tumour zones ~extracellular and intracellular fuchsinophilic bodies demonstrating an affinity for acidic dye fuchsin may be discerned which can be highlighted by smooth muscle actin (SMA) stain [4,5]. Upon ultrastructural examination, rough endoplasmic reticulum and cisternae may be discerned intracellularly along with few smooth muscle varieties of myofilaments. Besides, subplasmalemmal densities, plasmalemmal caveolae and external lamina confined within cell surface are observed. The constituent cells lack fibronexus junctions which are typically delineated within myofibroblasts. ‘Amianthoid fibres’ denominate collagen fibrils characteristically demonstrating a diameter of 50 nanometres to 83 nanometres, in contrast to giant collagen fibrils configuring true amianthoid fibres [5,6].
Figure 1: Intranodal palisaded myofibroblastoma depicting bland, spindle shaped cells with nuclear palisading with focal haemorrhage, amianthoid fibres and peripheral amalgamation of nodal tissue.
Figure 2: Intranodal palisaded myofibroblastoma exhibiting uniform spindle shaped cells with nuclear palisading, focal haemorrhage, amianthoid fibres and peripheral amalgamation of nodal tissue.
Spindle shaped cells constituting intranodal palisaded myofibroblastoma appear immune reactive to smooth muscle actin (SMA), vimentin, cyclin D1 or factor XIIIa. The amianthoid fibres may be highlighted with elastic stains, trichrome stain or smooth muscle actin (SMA) wherein type I collagen fibres appear confined to centric fibres and type III collagen fibres appear confined to periphery of amianthoid fibres [5,6]. Intranodal palisaded myofibroblastoma is immune non-reactive to S100 protein, synaptophysin, glial fibrillary acidic protein (GFAP), CD34, human melanoma black 45(HMB45) antigen, desmin, keratin and epithelial membrane antigen (EMA). Ki67 proliferative index is <5% [6,7]. Intranodal palisaded myofibroblastoma requires segregation from neoplasms as benign metastasizing leiomyoma, schwannoma, leiomyosarcoma, malignant melanoma, follicular dendritic cell sarcoma, Kaposi’s sarcoma, diverse carcinomas or sarcomas metastatic to regional lymph nodes, spindle cell carcinoma or spindle cell variant of malignant melanoma with metastasis into regional lymph nodes [6,7]. Intranodal palisaded myofibroblastoma can be appropriately alleviated with simple or localized surgical eradication of the neoplasm. Localized tumour reoccurrence is exceptional and distant metastasis remains undocumented [6,7].
CONCLUSION
Intranodal palisaded myofibroblastoma appear immune reactive to smooth muscle actin(SMA), vimentin, cyclin D1 or factor XIIIa and immune non-reactive to S100 protein, synaptophysin, glial fibrillary acidic protein(GFAP), CD34, human melanoma black 45 (HMB45) antigen, desmin, keratin or epithelial membrane antigen(EMA). Intranodal palisaded myofibroblastoma requires segregation from neoplasms as benign metastasizing leiomyoma, schwannoma, leiomyosarcoma, malignant melanoma, follicular dendritic cell sarcoma, Kaposi’s sarcoma, diverse carcinomas or sarcomas metastatic to regional lymph nodes, spindle cell carcinoma or spindle cell variant of malignant melanoma with metastasis into regional lymph nodes. Tumefaction can be appropriately alleviated with simple or localized surgical eradication of the neoplasm.
REFERENCES
- Weiss SW, Gnepp DR, Bratthauer GL. (1989). Palisaded myofibroblastoma. A benign mesenchymal tumor of lymph node. Am J Surg Pathol. 13(5):341-346.
- Suster S, Rosai J. (1989). Intranodal hemorrhagic spindle-cell tumor with "amianthoid" fibers. Report of six cases of a distinctive mesenchymal neoplasm of the inguinal region that simulates Kaposi's sarcoma. Am J Surg Pathol. 13(5):347-357.
- Kontosis A, Valanikas E, Papavramidis T, Koletsa T. (2021). Intranodal palisaded myofibroblastoma expressing DOG1: focusing on the potential diagnostic pitfalls. Rom J Morphol Embryol. 62(3):849-853.
- Haddad A, Marwan K. (2021). Intranodal Palisaded Myofibroblastoma: A Diagnostic Differential for Inguinal Lymphadenopathy. Am J Case Rep. 22:e934752.
- Wang XJ, Lin J, Bao XL, Liu X. (2022). Senile intranodal palisaded myofibroblastoma: report of a case. Zhonghua Bing Li Xue Za Zhi. 51(3):240-242.
- Bouhajja L, Jouini R, Khayat O, Koubâa W, Mbarek C, Ben Brahim E, et al. (2017). Intranodal Palisaded Myofibroblastoma in a Submandibular Lymph Node. Case Rep Otolaryngol. 2017:7121485.
- Laskin WB, Lasota JP, Fetsch JF, Felisiak-Golabek A, Wang ZF, Miettinen M, et al. (2015). Intranodal palisaded myofibroblastoma: another mesenchymal neoplasm with CTNNB1 (β-catenin gene) mutations: clinicopathologic, immunohistochemical, and molecular genetic study of 18. Am J Surg Pathol. 39(2):197-205.
 Abstract
Abstract  PDF
PDF